
Give them independence from med dependence
Half of men surveyed report dissatisfaction with BPH medications.ι The UroLift™ System offers rapid symptom relief, significant improvement in quality of life, and may enable patients to discontinue BPH meds.ιι, ιιι
Accelerate Your BPH Patients’ Path to Better Living

For decades, treating BPH has meant making a hard choice between medications, which may have bothersome side effects,8 or surgical treatment, with risk of sexual dysfunction.10
Now you can change a patient’s journey with confidence. The UroLift™ System can help men get off BPH medications and avoid major surgery.2 This straightforward procedure provides rapid symptom relief and recovery3,4 and preserves sexual function.*2
AUA BPH Guideline Recognize the Need for Earlier Intervention
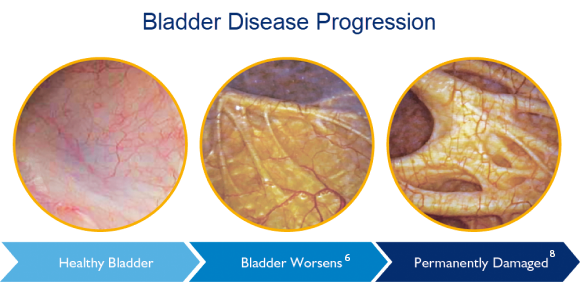
“Since many men discontinue medical therapy, yet proportionately few seek surgery, there is a large clinical need for an effective treatment that is less invasive than surgery. With this treatment class, perhaps a significant portion of men with BOO [bladder outlet obstruction] who have stopped medical therapy can be treated prior to impending bladder dysfunction.5”
The UroLift™ System is part of the standard of care for BPH treatment.5
What is UroLift™?
The UroLift™ System is the only leading enlarged prostate procedure that does not require heating, cutting, removal, or destruction of prostate tissue.3,10
Treatment with the UroLift™ System can be performed as a same-day outpatient procedure, including the office setting, under local anesthesia.4 It does not preclude future BPH treatments, should they be necessary.2
Safety
Risk profile better than reported for surgical procedures such as TURP3,8,9
Efficacy
Rapid symptom relief and recovery3,4 with no new, sustained erectile or ejaculatory dysfunction*10,12
Proven Durability
Proven to achieve sustained improvements in IPSS, QoL, and Qmax through 5 years2
Zero Day Global
The UroLift™ System is covered by Medicare, national, and commercial plans, when medical criteria are met. It is the only minimally invasive BPH procedure that has a zero day global.
Faster Recovery. Fewer Risks. Proven Outcomes.2,4,8,10
Patient Experience
Lowest rate of complications at one year when compared to both minimally invasive and invasive procedures.**14
89%
of obstructive median lobe patients would recommend the procedure at 1 month11
Durable Results
Improvements in symptoms, urinary flow, and quality of life sustained through 5 years2 with a retreatment rate of 13.5% at 5 years.2,3
50%
improvement in quality of life sustained over a 5 year study2
Preservation of Sexual Function
The only leading BPH procedure shown not to cause new and lasting sexual dysfunction.*10,12
0%
ejaculatory and erectile dysfunction*2
The Right Solution for Many BPH Patients
The UroLift™ System provides consistent outcomes to a broad range of BPH patients.13
| Prostate Indications for the UroLift™ System✝ |
| Minimum prostate volume | None |
| Maximum prostate volume | 100 cc |
| Obstructive median lobe | Yes |
The UroLift™ System Real World Retrospective Registry demonstrates that patients outside of the norm seen in clinical trials can be treated safely and effectively.13
- Younger patients
- Patients in retention
- Prostates <30cc
- History of prostate cancer treatment
- Diabetic patients
What are doctors saying?

Peer Perspectives
Learn about the latest clinical developments from your peers.
For Primary Care Physicians
Discover how the UroLift™ System fits into BPH care pathways.
View Resources
Find helpful information on how to build the UroLift™ System into your practice and continuing education opportunities.
References
1. U.S. 2022 estimates based on US Market Model 2022-24 (5-17-22 FINAL), which is in part based on Symphony Health PatientSource® 2018-21, as is and with no representations/ warranties, including accuracy or completeness.
2. Roehrborn, Can J Urol 2017
3. Roehrborn, J Urology 2013
4. Shore, Can J Urol 2014
5. AUA Guidelines 2021
6. Flanigan, J Urol 1998
7. Tubaro, Drugs Aging 2003
8. Sonksen, Eur Urol 2015
9. AUA BPH Guidelines 2003
10. AUA BPH Guidelines 2003, 2020
11. Rukstalis, Prostate Cancer Prostatic Dis 2018
12. McVary, Urology 2019
13. Eure, J Endourol 2019
14. Kaplan, Prostate Cancer Prostatic Dis 2023
15. Management estimate based on product sales as of June 2024. Data on file Teleflex Interventional Urology
† Food and Drug Administration (FDA) patient criteria for the UroLift™ System
*No instances of new, sustained erectile or ejaculatory dysfunction in the L.I.F.T. pivotal study
**Procedural complications were defined as complications requiring a return procedure in the outpatient setting ≥1d post-procedure
+ Paid consultant of Teleflex Interventional Urology
MAC12000-00 Rev A
