

Hearing Nothing Doesn't Mean Nothing's Happening
Are your patients still on BPH meds?
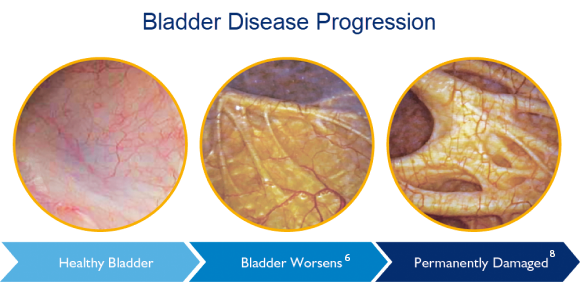
They may be silently suffering. Intervening earlier with treatments that address the blockage may preserve bladder health.6 Partner with UroLift-trained urologists in your area to support a faster care pathway.
Are you frustrated by medication nonadherence and the challenges of polypharmacy?
About half of men surveyed are dissatisfied with their BPH medication.3
Up to 71% of patients are non-adherent with their BPH meds after one year.4
Of men on BPH medications experience <4 point IPSS symptom improvement5
Help Your Patients Preserve Bladder Health
Impact on wellbeing
Quality of life and overall health are important considerations in treating men with BPH. Watchful waiting can risk long-term bladder health.6 The use of BPH medications may be associated with potential side effects,7 and many men are dissatisfied with the effectiveness of their BPH medication in relieving symptoms.3,5
“Since many men discontinue medical therapy, yet proportionately few seek surgery, there is a large clinical need for an effective treatment that is less invasive than surgery.”
The UroLift™ System Advantage
A mechanical solution to a mechanical problem
The UroLift™ System uses a proven approach to treating BPH that lifts and holds the enlarged prostate tissue out of the way, so it no longer blocks the urethra. It is the leading transurethral BPH treatment that does not require heating, cutting or removal of the prostate tissue.13,14 Post-procedure, most patients do not require ongoing BPH medications.15
Refer your appropriate patients to a urologist who can determine if they are a candidate for the UroLift™ System.
The UroLift™ System reopens the channel—with no cutting or burning of the prostate.
Common Questions Your Patients May Ask
What’s the harm in watchful waiting?
87% of men who elect watchful waiting reported a worsening of symptoms over a 4-year period.9
Can I continue taking my BPH medications forever?
Some BPH medications have been associated with serious issues, such as increased risk of cardiac failure and impaired cognitive function.1,2,10
What about sexual function?
UroLift™ System patients reported better outcomes in sexual function* and satisfaction than men who received BPH medication.12
Connect with a Teleflex representative to learn more and get resources for your staff and patients.
Download an IPSS form to help identify patients who may benefit from the UroLift™ System treatment.

Review the Clinical Data
Data from 145 peer-reviewed and 22 sponsored publications about the UroLift™ System.
Learn MoreGet Patient Perspectives
Watch videos and read blogs about real-life experience with the UroLift System.
Learn MoreBPH Advisor
Patients can take a short quiz to get a personalized, detailed BPH report and receive helpful articles by text or email.
Learn MoreReferences
1. Duan, Pharmacoepidemiol Drug Saf 2018
2. Welk, J Neurol Sci 2017
3. Survey of US men aged 40+ who have been diagnosed with BPH (enlarged prostate) and are/have been treated with BPH medications, conducted by Teleflex in 2020. Data on file, n=96.
4. Cindolo, Eur Urol 2015
5. Wei, et al, 2010 Abstract
6. Flanigan, J Urol 1998
7. AUA Guidelines 2003
8. Tubaro, Drugs Aging 2003
9. Djavan, Urology 2004
10. Lusty, J Urol 2021
12. Roehrborn, Eur Urol Focus 2021
13. Roehrborn, J Urol 2013
14. AUA Guidelines 2003, 2020
15. Roehrborn, Can J Urol 2017
*Based on an indirect comparison of erectile and ejaculatory function and sexual satisfaction in men who received PUL in controlled studies or in men who received medical therapy in the MTOPS study.
+ Dr. Robert Cowles was previously a paid consultant of Teleflex
MAC03180-01 Rev A